Populism does not help public health
Relevance: GS II (Social Justice and Governance)
- Prelims: POSHAN Abhiyan Scheme;
- Mains: Health Care System in India; Challenges associated with Health System and Governance;
Why in the News?
A degree of autonomy is needed in public health decision-making to ensure policies are aligned with the people's immediate and practical needs while striking a balance between expert-driven decisions and public aspirations.
Challenges faced by India's Public Health System
- Lack of awareness: Low educational status, poor functional literacy, and low priority for health in the healthcare system contribute to a lack of awareness about health issues and preventive measures.
- The absence of specialized courses such as public health engineering in India’s educational institutions points to a gap in the multidisciplinary approach required in public health management.
- Public health is not just about treating diseases. It is about preventing them, requiring expertise from various fields such as environmental science, sociology, urban planning, and economics.
- The current physician-centric focus of India’s public health system often fails to capture this comprehensive nature.
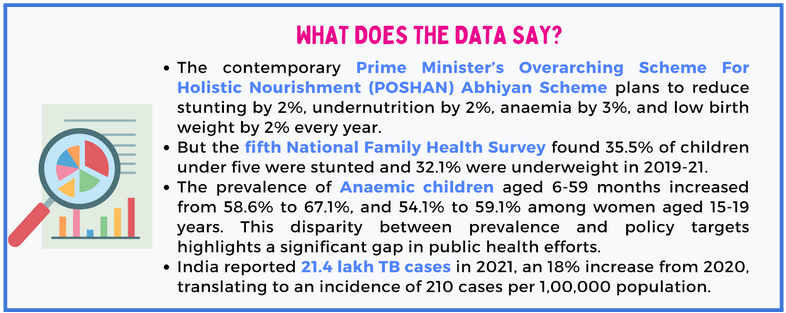
- Populist tendencies: Behavioral change is key to managing public health challenges. Yet, it can be challenging in political environments influenced by populist tendencies.
- In particular, political leaders across the spectrum have leaned towards initiatives that promise immediate results, such as new hospitals, subsidized treatments in private hospitals, emergency response (over preventive response), and populist health policies.
- Many of these measures do not have much of an impact because of a lack of action beyond public announcements, which is almost always due to budgetary constraints.
- But even before being implemented, these schemes and the focus of our leaders on them divert attention from critical areas such as sanitation, disease surveillance, and public health education, which are important to maintain population health and prevent disease outbreaks.
- Inadequate funding: The percentage of total government expenditure on healthcare in India is lower compared to other countries, leading to inadequate funding for the healthcare sector.
- The United States reported only 8,331 TB cases in 2022, about 2.5 cases per 1,00,000 persons.
- This disparity is not merely a matter of the availability of medical treatment but is deeply linked to socio-economic factors such as poverty, sanitation, and overcrowding (as a result of poorly organised urban housing) prevalent in India.
- Disparities in health and healthcare systems: There are significant differences in health and healthcare systems between poorer and richer states, leading to unequal access to healthcare services.
- In India’s bustling cities and tranquil villages, there is a silent but significant fight raging on the public health front. It is diseases such as smallpox (though eradicated, it is still under surveillance), polio, neonatal tetanus, and measles, through improved sanitation and vaccines.
- These are unsung wins where the absence of illness speaks volumes. Yet, in a democratic setup, leaders often chase tangible achievements and, inadvertently or otherwise, overlook these vital preventive efforts.
- Negligence of public health functions: Due to inadequate funding, public health functions are often neglected, leading to a lack of focus on preventive measures and disease surveillance. The increasing burden of chronic diseases, such as obesity, diabetes, and tobacco use, requires a more comprehensive approach to healthcare.
- Limited government-financed health insurance programs: While new health policies and schemes have been introduced, insurance remains limited, and many Indians, especially the poor, continue to receive unacceptably low-quality primary and hospital care.
- Research and development in these areas are crucial. For example, despite its limitations and restrictions, the existing dengue vaccine underscores the need for more research. Climate change is also affecting mosquito breeding and movement patterns, and public health strategies need to adapt to these changes.
- Civil servant Joseph Bhore’s insights from 1946, into the economic and human cost of neglecting preventive health measures, still ring true. Investments in nutrition programmes, while not immediately visible, have far-reaching implications for health and productivity.
|
The case of dengue
|
Why is a degree of Autonomy needed?
A degree of autonomy is needed in India's public health system to address the challenges faced by the system. Here are some points highlighting the need for autonomy:
- Improved management performance: Autonomy in facility-level management can lead to better performance in primary healthcare facilities, ultimately enhancing the quality of services.
- Public health decisions should be based on scientific evidence and long-term goals rather than short-term political interests. This separation will ensure public health policies are driven by data and expertise, not electoral cycles.
- Tailored decision-making: Autonomy allows local health authorities to make decisions that are more aligned with the specific needs of their communities, addressing disparities in health and healthcare systems.
- A fair and effective health system requires freedom from political influence, focusing on policymaking and implementation driven by scientific evidence and long-term objectives.
- While prioritising health decisions based on scientific evidence and overarching public health goals are crucial, there is a risk of disconnecting from the immediate health concerns of the general populace.
- Decentralized approach: India's decentralized approach to healthcare delivery necessitates a certain degree of autonomy to ensure that decisions are tailored to local needs and resources.
- Effective public health management should encompass preventive measures, policy formulation, community health, and environmental health, among others. In public health, adopting a separation of powers approach is essential.
- To address this, an ideal solution would be to place Health Ministries directly under the leadership of elected officials, such as the Chief Minister or the Prime Minister, similar to the management of the space and the atomic energy departments.
- This structure would not only provide a degree of autonomy but also ensure that health policies are aligned with the people’s immediate and practical needs, striking a balance between expert-driven decisions and public aspirations.
- Public health policies: Autonomy can help prioritize public health policies and incorporate more public health policies and diverse perspectives in the healthcare system.
- Infectious diseases, non-communicable diseases, health-care access, mental health, and misinformation pose challenges that demand a more holistic, long-term approach in public health policy.
- Collaboration with international organizations: Autonomy can facilitate collaboration with international public health organizations to gather more knowledge and expertise in the field.
- Education and training: Autonomy can help address the gap in education about public health among officials in policy-making positions and promote the development of Master of Public Health (MPH) and PhD programs in public health.
- Transparency: Autonomy can ensure that research findings are made transparent to the Indian public, promoting evidence-based decision-making and policy development.
- A fair and effective health system requires freedom from political influence, focusing on policymaking and implementation driven by scientific evidence and long-term objectives.
Way Forward:
- Providing a degree of autonomy in India's public health system can lead to improved decision-making, better management performance, and a more tailored approach to addressing the diverse healthcare needs across the country.
- To address these challenges, India needs to prioritize public health, increase funding for healthcare, and focus on preventive measures and disease surveillance.
- This can be achieved through a combination of government policies, community-based interventions, and public health education programs.
Mains PYQ
Q. Appropriate local community level healthcare intervention is a prerequisite to achieve ‘Health for All’ in India. Explain. (UPSC 2018)
Q. Professor Amartya Sen has advocated important reforms in the realms of primary education and primary health care. What are your suggestions to improve their status and performance? (UPSC 2016)