Relevance: GS II (Social Justice)
News Excerpt:
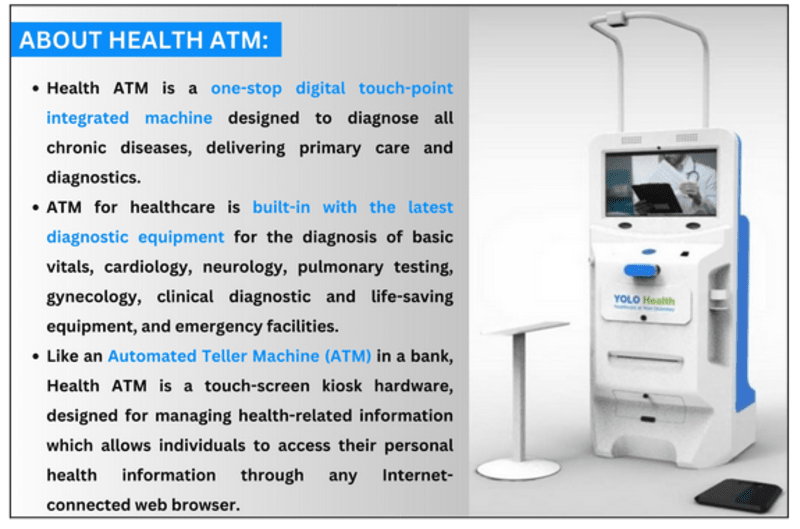
The Health ATMs were launched by Karnataka Chief Minister Siddaramaiah during the Kalyana Utsav in rural areas as a first-of-its-kind effort in the state.
Significance of Health ATMs:
-
For Patients: It allows patients to be more empowered and allows them to actively participate in managing their health needs with access to world-class medical facilities.
-
For Local Health System: It resolves the problems of primary health services in rural and remote areas. It’s a modern, sophisticated, simplified, accurate & automated healthcare kiosk.
-
For better recognition: The multifaceted machine helps in the easy diagnosis of medical problems for people in remote locations, where hospitals are not within reach. It also provides a central platform for the patients to interact with specialists in the fields through Telemedicine (E.g.- Video conferencing).
Challenges for Indian Rural Health Care Services:
-
Shortage of infrastructure: Currently, India has just 25,743 Primary Health Care Centers (PHC) and 5,624 Centers for Health Care Strategies (CHCS) against the estimated need for 29,337 PHC centers and 7,322 CHCS.
-
Hence, due to the high demand and low availability of Primary Health Centers and Community Health Centers (CHCs), an average facility is serving many more people than it is equipped to serve.
-
Lack of Human resources and specialized personnel: According to the Rural Health Statistics 2019-20, there is a shortfall of 76.1% specialists at the CHCs as compared to the requirement for existing CHCs. Altogether, 56,581 positions of doctors and other health staff are vacant in rural areas.
-
Less Funding by Government: India spends way too little on health in comparison to other developed nations like the U.S. and Japan. However, the Economic Survey 2020-21 has strongly recommended an increase in investment in public healthcare services from the present 1% to at least 2.5-3% of the GDP.
-
Unaware public and behavioral issues: Due to a lack of education, vaccine hesitancy was seen among the rural population during the COVID-19 pandemic. Rural masses are not aware of the health services being provided under several health schemes which impacts the efficacy of such schemes.
Way Forward:
-
Need for Integrated and Detailed Healthcare Management: Appropriate utilization of resources at primary health facilities reduces the burden at the secondary and tertiary levels of care by reducing unnecessary referrals.
-
Need for maintaining database: The data and information need to be available with rural health networks to monitor the health indices of the population at the very primary level itself.
-
Updating Rural healthcare with emerging Technologies: Telehealthcare centers can be used to increase access to specialist prescriptions from nearby PHCs.
-
For example, ICMR’s Arogyasri is a mobile-based app that integrates multiple hospitals, medical specialists, and available rural clinics as well.
-
Need to increase citizen participation: In a cross-country analysis of governance systems and health outcomes, countries with robust local governments were found to have consistently lower infant mortality rates than those with more centralized forms.
-
In West Bengal and Kerala where primary healthcare is co-managed by Panchayats, the health outcomes are far more better than the other states.
PYQs
Q1). Professor Amartya Sen has advocated important reforms in the realms of primary education and primary health care. What are your suggestions to improve their status and performance? (2016)
Q2). Smart cities in India cannot be sustained without smart villages. Discuss this statement in the backdrop of rural-urban integration. (2015)
